The full and equal participation of women in science is vital to achieving gender equity and advancing progress in global health. Unfortunately, today less than 30 percent of the world’s researchers are women, and female researchers tend to have shorter, less well-paid careers and to see their work underrepresented in top journals.
This gender gap has far-reaching implications. Health and gender are inextricably linked. For example, women and girls are at increased risk of a number of poverty-related and neglected diseases (PRNDs), due both to biology and to nonbiological factors like discrimination and gender power dynamics. Women can also feel disproportionate impacts of illness due to wider consequences like stigma, reproductive, financial, and social effects. To meet the health needs of women and girls and better facilitate the integration of sex and gender considerations at all levels of medical research, it’s imperative that women be better represented in leadership and decision-making ranks within research teams.
In recognition of International Day of Women and Girls in Science, which aims to inspire and engage more women and girls in science, GHTC is profiling five fierce female innovators who have transformed global health research.
1. Dr. Ruth Bishop, discoverer of rotavirus
 Photo: Stepping Stone Pictures
Photo: Stepping Stone PicturesAs a young bacteriologist working in the 1970s, Dr. Ruth Bishop was on a quest to find the root cause of diarrheal disease—the most common cause of illness and the second leading cause of death among children worldwide. After much research, Ruth concluded that the disease was likely not caused by a bacterial agent, but instead by a virus.
To continue her search, Ruth teamed up with colleagues at the University of Melbourne. In 1973, using an electron microscope, the team uncovered a previously unidentified virus in the biopsy sample from an intestinal lining. Ruth and her team went on to confirm presence of the virus in other samples. Their published results elicited a global response and confirmation of the virus’s presence in samples around the globe. The virus identified by Ruth and her team would come to be named rotavirus for its wheel-like shape. Rotavirus is the leading cause of severe diarrhea in children worldwide and the cause of about one-third of all diarrheal-related child deaths.
Ruth and her team subsequently developed a diagnostic test for the rotavirus, and their continued research helped pave the way for the development of a rotavirus vaccine, which was first introduced more than three decades after her initial discovery. Gavi, the Vaccine Alliance, estimates that by 2030, 2.4 million lives could be saved through rotavirus immunization. Ruth is now retired, but her legacy lives on in the millions of children’s lives that have been saved by her discovery.
2. Dr. Quarraisha Abdool Karim, pioneered use of antiretrovirals to prevent HIV and research on broadly neutralizing antibodies
 Photo: UNAIDS
Photo: UNAIDSAs a native of South Africa and infectious disease epidemiologist, Dr. Quarraisha Abdool Karim saw the devastating impact HIV/AIDS was having on her home nation, where one out of every five people in the world with HIV lives. While there were many research efforts focused on fighting the growing epidemic, Quarraisha felt too little attention was paid to the disproportionate burden young women bore in the epidemic and solutions to address that. So Quarraisha and her husband, Dr. Salim Abdool Karim, in 2001 brought together a group of top HIV researchers to form the Center for the AIDS Program of Research in South Africa (CAPRISA), which is today regarded as one of the most influential AIDS research programs in the world.
In 2010, CAPRISA completed a landmark study proving for the first time that a microbicide gel, using the drug tenofovir—normally used as an antiretroviral to treat HIV/AIDS—could offer some protection from the virus when used before and after sex. While today the field has moved on to other prevention methods like daily pills and long-acting injectables, this research provided the first proof-of-concept that antiretrovirals could be used to prevent, as well as treat, HIV in women and built the foundation for the approach known today as pre-exposure prophylaxis (PrEP), which is widely used globally to prevent HIV infection. CAPRISA research has also led to the development of “broadly neutralizing antibodies,” after it was discovered in 2012 that an HIV-positive woman in one of the center’s studies produced unique antibodies that not only attacked the strain of HIV she had, but also 80 percent of other known HIV strains circulating globally. The isolation and recreation of these antibodies in a lab has led to a growing field of study that could one day lead to longer-acting HIV treatments and pave the way to the ultimate goal of an HIV vaccine.
Reflecting on her career, Quarraisha said, “I’ve spent three decades working on preventing HIV infection in young women. Progress has been made, but it’s far from complete. We need interventions that can meet the diverse needs of vulnerable women.”
3. Dr. Kizzmekia Corbett, co-developer of Moderna-NIH COVID-19 vaccine
 Photo: University of Maryland Baltimore County/Marlayna Demond
Photo: University of Maryland Baltimore County/Marlayna DemondAs a high school student growing up in North Carolina, Dr. Kizzmekia Corbett knew she wanted to be a scientist, but it was a chemistry internship program for gifted minority students that put her on the path to becoming one of the US government’s lead coronavirus vaccine researchers at a pivotal moment in history. This high school internship program in lab led Kizzmekia to an undergraduate scholarship to study biology and sociology, which in turn led her to a PhD in microbiology and immunology, which ultimately landed Kizzmekia a research fellowship and then job at the US National Institutes of Health’s (NIH) Vaccine Research Center.
It was there, on the coronavirus research team, that Kizzmekia found herself in January 2020 when her team first got word of outbreak of an unknown respiratory disease in Wuhan, China, that would later be identified and known as COVID-19. Kizzmekia and her team quickly got to work on trying to develop a preventative vaccine. Applying earlier research she has conducted on making coronavirus spike proteins stabilized in a way that enables the immune system to mount a stronger response and partnering with the biotech company Moderna to use its messenger RNA (mRNA) platform, the research team was able to advance a vaccine candidate into phase 1 clinical trials just 66 days after the virus sequence was released. In a triumph of science, nine months later, on December 18, 2020, the vaccine was authorized for emergency use in adults by the US Food and Drug Administration. While much unfinished work remains to ensure coronavirus vaccines reach everyone worldwide, Kizzmekia has said of her scientific accomplishments, “To be living in this moment where I have the opportunity to work on something that has imminent global importance…it's just a surreal moment for me.”
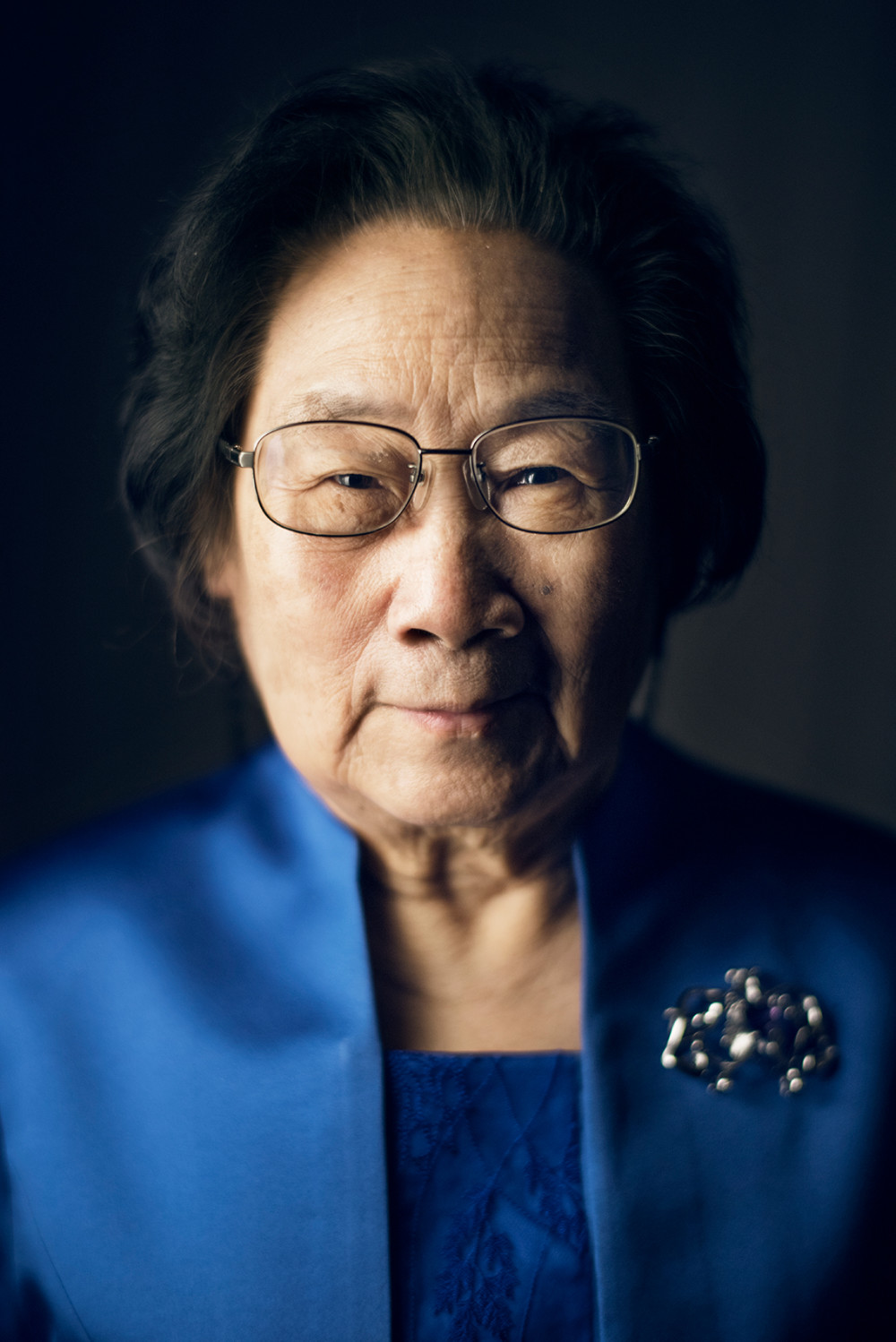
4. Dr. Tu Youyou, discoverer of artemisinin, a key ingredient in modern malaria medicines
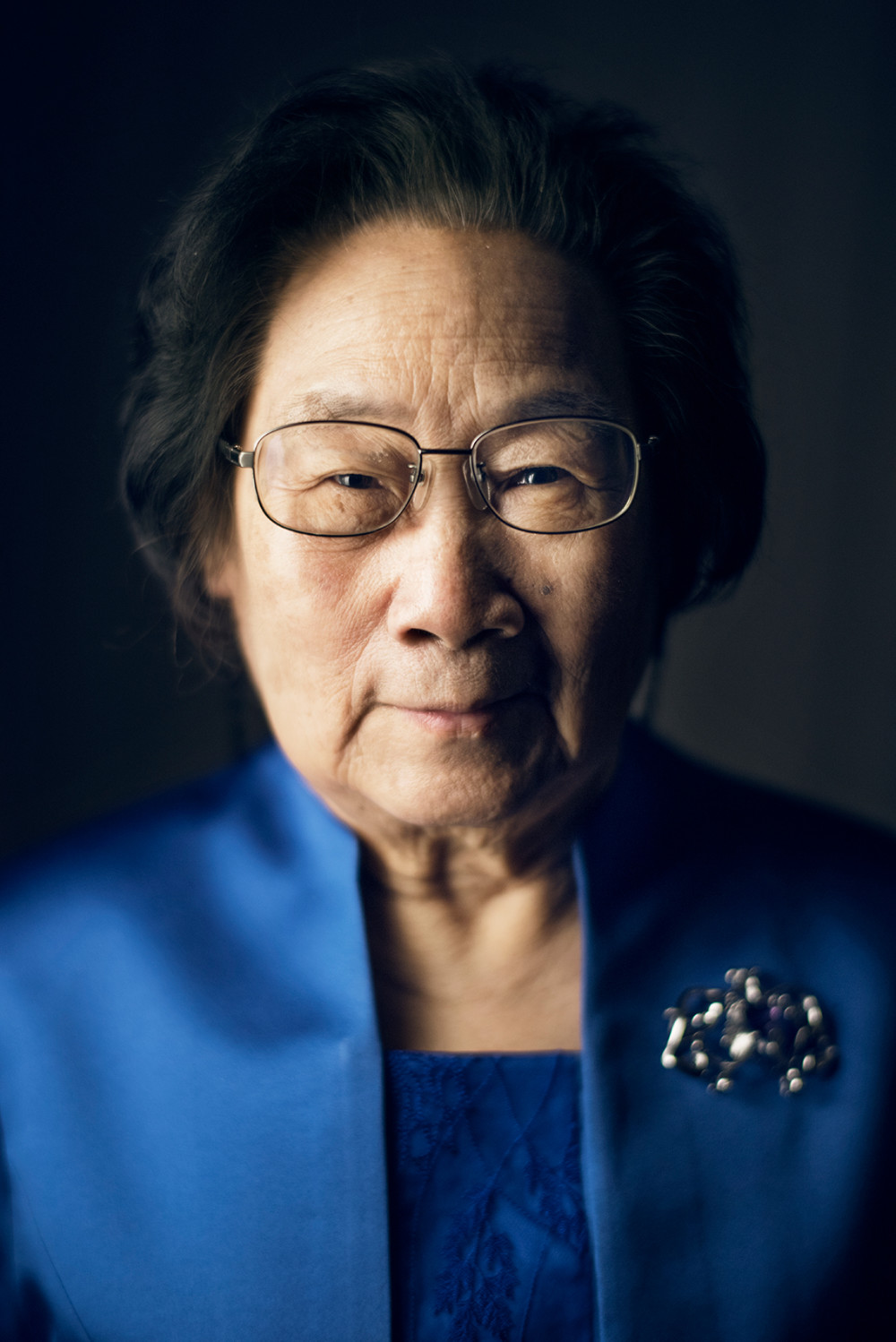 Photo: Nobel Prize/A Mahmoud
Photo: Nobel Prize/A MahmoudDr. Tu Youyou was born into a family that valued education, but it was a two-year battle with tuberculosis at the age of sixteen that inspired her to study medicine, so she could find cures for diseases like the one that affected her. After pursuing a degree in pharmacology, with an emphasis on the study of medicinal plants, Tu went on to work at a newly established academy devoted to studying traditional Chinese medicines applying modern research methods. In 1967, Tu was put in charge of an ambitious Chinese government project to find a new cure for malaria, which had become resistant to chloroquine, the standard treatment at the time.
In her quest to find a cure, Tu and her team turned their attention to ancient Chinese medical texts, where the team found reference dating back to around 400 A.D. to the use of sweet wormwood to treat fevers associated with malaria. In 1971, Tu and her team isolated one of the compounds from the plant that they believed to have malaria-fighting properties, but after testing it, saw inconsistent results. The team was about to abandon that line of research when Tu had a vital insight: the extraction process used, which involved boiling the plant in water, could be negatively impacting the compound’s medicinal properties. Tu decided to instead use an extraction method with ethyl ether, which boils at a lower temperature. The results were stunning: the compound showed a 100 percent success rate in animal testing and the first 21 patients it was tested on all recovered.
The compound Tu and her team isolated—artemisinin—and its derivatives are the basis of combination therapies that are today the gold standard treatment for malaria. In 2015, Tu was awarded a Nobel Prize for her discovery, which she called “a gift from traditional Chinese medicine to the world.”
5. Dr. Monique Wasunna, researcher of new treatments for neglected tropical diseases
 Photo: KfW
Photo: KfWDr. Monique Wasunna, a native of Uganda, grew up in an era when girls were expected to remain in the domestic sphere, but her father’s belief in the power of education and his commitment to advancing equal gender roles in the household helped her realize she could enjoy a different future. While a teen, Monique’s younger sister became severely ill and hospitalized due to measles, and this experience inspired Monique to pursue a career in medicine.
For more than 30 years now, Monique has been working to advance treatments for the world’s most neglected patients, most notably as the former long-serving director of the Center for Clinical Research at the Kenya Medical Research Institute and currently as director of the Drugs for Neglected Diseases initiative’s (DNDi) Africa office. Over the course of her career, Monique has been a principal investigator on numerous clinical trials to find better treatment options for neglected diseases and has spearheaded new partnerships to expand clinical trial capacities in the East African region. Her work with DNDi has helped the organization advance several groundbreaking new treatments for neglected tropical diseases, including an improved, affordable therapy for leishmaniasis, which reduced treatment time from 30 days down to 17, and an all-oral cure for sleeping sickness.
Monique believes that health is a human right, and that innovation is vital to delivering better health for all. As the world confronts global health challenges, “the most important thing is that we leave no one behind,” Monique said.
For a broader look at the gender-related aspects of PRNDs and how policymakers can improve gender equity in global health research, check out this study from DSW.