In this guest post, Lindsay McKenna, TB/HIV project officer at GHTC member Treatment Action Group (TAG), writes about a newly released report examining advancements in tuberculosis (TB) research and development (R&D).
TAG’s 2015 Pipeline Report looks at advances in diagnostics, treatment, and prevention that offer
hope for those engaged in the global fight against TB. The report, which also covers HIV and hepatitis C, highlights scientific potential
while recognizing that the realization of innovations in the pipeline is conditional on our ability to mobilize political will, resources, and collaboration.
Indeed, the direction of TB R&D is positive relative only to decades of stagnation, which has resulted in lengthy therapy, a lack of options for
treating children, cumbersome diagnostics, and a vaccine of waning efficacy. Improved tools are therefore not only possible, but urgently needed. This
article highlights key findings from the report and its recommendations for researchers, funders, regulators, and advocates to ensure continued and
accelerated progress.
The TB treatment pipeline: moving beyond “making the most of what we’ve got”
TB treatment researchers are making progress, though it is slow. There are few new TB drug candidates and limited funding to develop them. A number of
advances to shorten preventive therapy for TB and evaluate the possibility of preventing multidrug-resistant TB (MDR-TB) offer potential for markedly
improving TB prevention, though they raise questions about implementation strategies. For active TB disease, studies to determine the best drug combinations,
dosing, and strategies to shorten treatment are ongoing and may answer long-standing questions. TRUNCATE-TB, a bold new design to shorten treatment
for drug-susceptible TB, will attempt to bring TB treatment for most cases down from six to just two months. Trials to test new drugs in better combinations
are at varying stages of development and, although results are still years away, offer the prospect of improved treatment for MDR-TB.
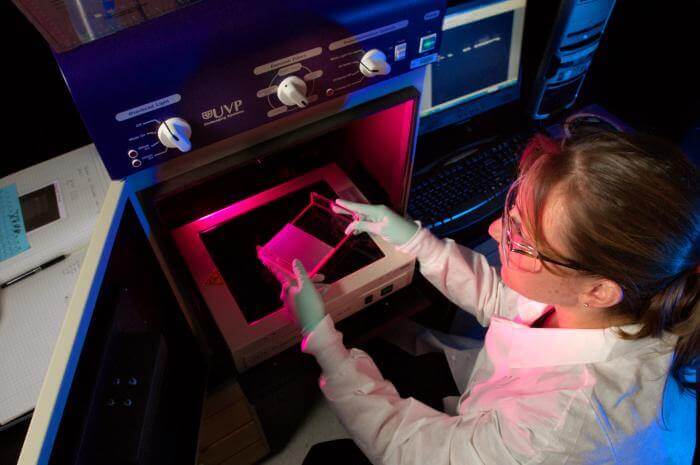
- CDC research studying drug-resistance. Photo: CDC/ Hsi Liu, Ph.D., MBA
While R&D is advancing for existing—and a few late-stage—TB drugs, the small number of new early-stage compounds, the lack of diversity
in the TB drug pipeline (i.e., only six compounds from three drug classes), and the slow pace at which they are progressing is worrisome. Furthermore,
access to new TB drugs and those used off-label for TB treatment remains a challenge for researchers, programs, and patients, slowing scientific advancements
and their impact on those in need of them.
To ensure the development and availability of improved treatments for TB, the 2015 Pipeline Report calls for increased funding for TB R&D,
wise investments of this funding, early planning for access to new treatments, and improved regulatory systems to facilitate adoption of innovations
once developed.
Momentum in the pediatric TB treatment pipeline

- Pediatric formulations of TB drugs are urgently needed. Photo: PATH/Gabe Bienczycki
Inadequacies in TB treatment are magnified for children, and major data gaps on TB treatment in children persist. However, research currently planned and
underway aims to optimize treatment with existing drugs and inform the use of new treatments for children with TB. A movement toward including children
at an earlier point in TB drug research may also help shorten the time between adult and pediatric approvals and improve access in the future.
Studies underway will evaluate preventive therapy in children exposed to MDR-TB and whether it is possible to shorten treatment for less severe forms of
TB and TB meningitis in children. Appropriately dosed pediatric formulations of first-line TB drugs are approaching market introduction, but those
for second-line and new drugs are farther behind. Much work remains to study regimens and new drugs in children and to develop missing pediatric formulations.
The 2015 Pipeline Report recommends earlier and expedited investigation of new drugs in children, in which both developers and stringent regulatory
authorities play an important role. The report also urges the immediate advancement of guidelines for and development of pediatric formulations of
second-line drugs. Increased investments in pediatric TB R&D will facilitate all of these important steps.
The TB diagnostics pipeline
We urgently need new diagnostic tests for TB. Fortunately, we now have a clearer-than-ever picture of what types of tests are most essential: a more effective
but low-tech test to replace smear microscopy in detecting TB, a rapid drug-susceptibility test to guide treatment, a biomarker test, and a triage
test. Yet the pipeline for TB diagnostic tools remains stagnant, with several products in line but little high-quality evidence being generated towards
an effective, accessible, point-of-care test.
Eiken TB-LAMP (loop-mediated isothermal amplification) and Alere Determine LAM (urine lipoarabinomannan lateral flow test) underwent World Health Organization (WHO) expert review and are awaiting decision. WHO review is expected
soon for Hain Lifescience MTBDRsl, a test to detect resistance to fluoroquinolones and injectable agents. Results were published for several
molecular diagnostic and drug-susceptibility test candidates, including Xpert MTB/RIF Ultra, a platform that claims improved sensitivity and ability
to detect isoniazid resistance. However, appropriate field evaluations and more evidence is required in order for any tests in the pipeline to be considered
for WHO expert review and to inform national TB program policies.
To improve detection of TB, the 2015 Pipeline Report recommends that we invest in TB R&D and diagnostics research, including for new biomarker-based
triage/point-of-care tests, and integrate TB diagnostics research into ongoing treatment studies. The report also argues that access to validated new
tests and to drug susceptibility testing should be universal, and linkages to treatment ensured. Countries and donors must prepare for the launch of
next-generation tests while eliminating the current use of inaccurate and misleading tests. As with drugs, regulatory capacity to oversee TB diagnostics
research needs improvement.
The TB vaccines pipeline: a new path to the same destination?
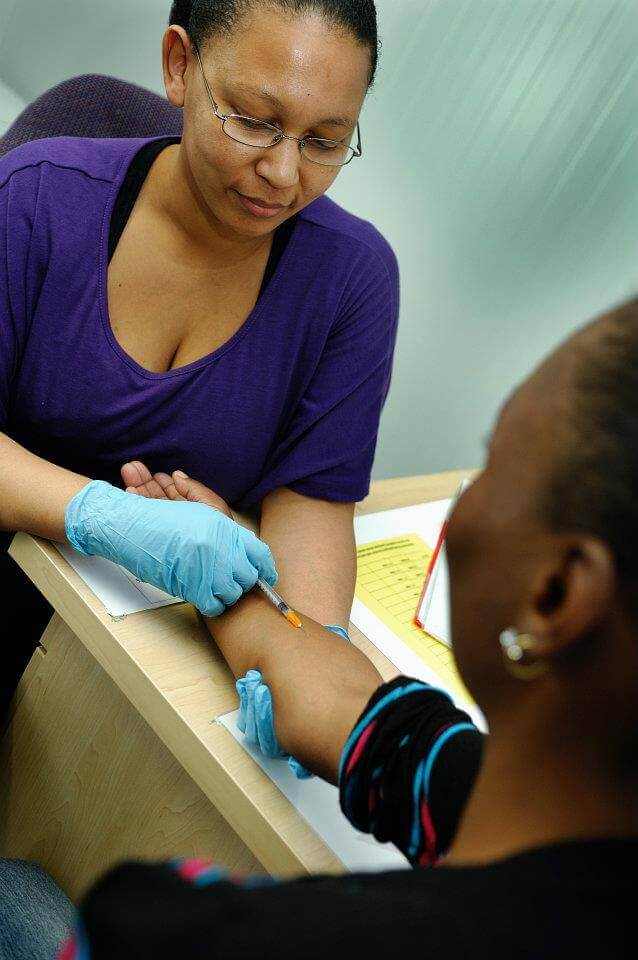
- A researcher conducting a vaccine clinical trial. Photo: AERAS
Attention and resources for TB vaccine R&D are moving away from late-stage clinical trials and back to basic discovery and preclinical science. Motivating
this welcome shift is emerging evidence that encourages a reexamination of the assumptions that have guided the last ten years of TB vaccine research.
Candidates in the current TB vaccines pipeline only contain a few of the vast number (4,500) of targetable antigens and focus on stimulating just one
of the many parts of the immune system. The shift “to the left” of the development pipeline will allow exploration of more vaccine concepts and help
to de-risk vaccine development.
The report highlights progress in basic science and preclinical development, including the pursuit of biomarkers of protective immunity to TB infection
or disease, the application of radiology to study immune activity against mycobacterium TB and to better understand host-pathogen interactions, and
vaccine design concepts to trigger robust cell-mediated immunity.
The development of a more efficacious vaccine with longer-lasting immunity will require us to: increase funding and support for basic science and create
opportunities for immunology work in clinical trials; establish meaningful partnerships with civil society organizations and TB-affected communities;
and be guided by principles of equity while preparing for access to future vaccines.